Dr Julia Del Amo: HIV-related issues in people with a migrant background

How did you come to be working in the field of HIV?
After training as a medical doctor in Spain, I went to the UK to train in infectious diseases, as there was (and still is) no infectious diseases specialization in Spain.
This was in the early 1990s at the height of the HIV epidemic. It was very shocking to witness so many young people with HIV dying; it really changed my life and that of many people of my generation.
What stimulated your interest in migrant-specific issues?
I was working at the Royal London Hospital in east London, which is an area with lots of migration. I noticed that the patients I was looking after, migrants from sub-Saharan Africa, had completely different issues to those of white gay men. So I started collecting information by hand from all the African people who attended the hospital and I realized they had a different clinical presentation, the need for prophylaxis was different, there were more women, there was mother-to-child transmission, and many other aspects that needed to be addressed.
At some point, I attended a lecture by Professor Kevin de Cock who described how he wanted to know more about what happened to Africans who migrated to Europe and how the patterns were changing, but that he had no data. After the lecture, I told him about the information I had collected on paper about African migrants in the London, upon which he invited me to do a PhD on the subject. It was a wonderful opportunity and since then, migrant health has remained my focus.
What were the problems facing Sub-Saharan African migrants at the time?
By the 1990s the gay community was well organized, but the African community was in huge denial. This denial, reflecting what was happening in their countries of origin, was very damaging to them. At the same time, mistakes were being made in the healthcare approach, because authorities were afraid of seeming racist in screening policies. For example, you couldn’t offer an HIV test to a woman from sub-Saharan Africa, because the policy didn’t recommend it for white women either. Although we knew very little then compared to now, we did know that of those women from sub-Saharan Africa, 25% were HIV positive and the likelihood of them transmitting HIV to their children was very high, unless we did something for them. Sadly, we weren’t responding to the issues because there was so much stigma that people were paralyzed about taking those decisions.
How has HIV among migrant populations in Europe changed over time?
In the 1990s the majority of migrants living with HIV in Europe had been infected in their countries of origin, although this was difficult to establish at the time because it requires a detailed migration history that many people were not willing to disclose.
Things have changed greatly in the last 15 years. Migrant communities have become established and people are now more likely to become infected in the country of destination, with infection then being further transmitted within the community. Of course, this varies greatly according to geographical origin. For example, in a recent aMASE study (funded by EuroCoord) we found that in Spain up to 70% of the new HIV infections in migrants are acquired post-migration. This is particularly true among men who have sex with men (MSM) from Latin America and the Caribbean, although we are also seeing more post-migration transmission among people from sub-Saharan Africa.
Why do you think we are seeing this rise in post-migration HIV infection among MSM?
It’s a complex question with no single answer. However, we think it is due to a combination of engaging in more unsafe sex and a higher HIV prevalence among MSM in Europe. We haven’t been able to test this hypothesis yet, though. To measure whether MSM are engaging in more unsafe sex post migration, we need to carry out surveys. In the aMASE study we did ask about sexual behaviour and sexual partners, but we need additional information about their sexual activity before migration.
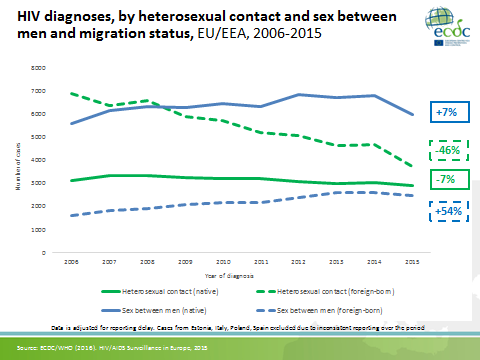
ECDC have also very recently separated out the HIV case-based surveillance data according to geographical origin and transmission category, and found that the number of migrant MSM is increasing, as well as the number of new HIV diagnoses among MSM.
What trends have been observed among migrants from sub-Saharan Africa?
For heterosexual Africans, the ECDC data show that the number of new HIV diagnoses in men has been declining systematically from 2005 onwards, and in women this decrease is even more pronounced. Unfortunately, though, we have very little information on undocumented migrants and the associated trends.
Why are the numbers of new HIV diagnoses declining among migrants from sub-Saharan Africa?
To understand why the numbers are declining, we need to do modeling work. My impression is that, as well as lower numbers of incoming migrants from sub-Saharan Africa due to migration restrictions, fewer HIV-positive people are also coming because the HIV incidence is declining in their country of origin. Moreover, in heterosexual epidemics, when you treat the index case the transmissibility decreases significantly. This makes heterosexual epidemics easier to manage than epidemics with multiple sex partners, like in the gay community.
What are your plans for future research?
As the number of migrant MSM is increasing all over Europe, I believe this should be our focus. There are specific issues among migrant MSM that need to be addressed, such as those relating to culture, language, access barriers and entitlement to care, and I think they should be considered through a multidisciplinary approach.
In addition, we are analyzing the most recent ECDC dataset to look at numbers of new HIV diagnoses in migrants, stratifying by region of origin and transmission category, but also looking more deeply into the different regions in Africa. We are also thinking about doing some modeling work to disentangle some of these questions. However, this is challenging. Firstly, it depends on what information each country can provide, because you need extensive migration data to make certain assumptions. Moreover, each European country has a very specific population of migrants, and, finally, there are no data available on undocumented migrants. So various factors are involved and I would like to quantify the contribution of each of these factors and draw conclusions to apply to other groups that are going to need interventions.
